Research Article - (2023) Volume 13, Issue 1
Received: 30-Jan-2023, Manuscript No. JBL-23-88186;
Editor assigned: 02-Feb-2023, Pre QC No. JBL-23-88186 (PQ);
Reviewed: 16-Feb-2023, QC No. JBL-23-88186;
Revised: 23-Feb-2023, Manuscript No. JBL-23-88186 (R);
Published:
02-Mar-2023
, DOI: 10.37421/ 2165-7831.2023.13.298
Citation: Timimi, Zahra AL. "The Function and Value of
Laser Pulsing Operation Mode in Wound Healing Therapy." L Blood Lymph 13(2023):298.
Copyright: © 2023 AL-Timimi Z. This is an open-access article distributed under the terms of the creative commons attribution license which permits unrestricted use,
distribution and reproduction in any medium, provided the original author and source are credited.
Despite having a basic grasp of laser wavelengths and dose ranges, there was no consensus on whether continuous mode or pulsing mode should be used, which is more dependable, and what determinants should be used to support the parameters of a pulsating laser. The molecular and cellular mechanisms of cold laser treatment have been investigated. The many types of pulsed lasers available have been described as the factors that influence the creation of their pulses. Investigations that were dissolved by continuous and/or pulsed laser modes were evaluated in vivo and in vitro. The laser therapy pulse repetition rates were matched. Several notable confirmations have shown that pulse mode has different effects on wound healing and damaged tissue than continuous mode. To completely assess the performance of cold laser treatment in cutaneous wounds healing, measurable clinical research that associates cellular effects in addition to biological processes is required. More research is needed to confirm these findings for a variety of wound types and treatments in a variety of settings, including pulsating mode structures. Future research should concentrate on well-controlled studies that rationally determine laser types and therapy parameters.
Wound healing • Pulsed • Laser therapy • Parameters • Repetition rates
A unique kind of laser known as cold laser influences biological systems without using heat. The research in this field began in 1967 with the effort of Mester, et al. They discussed how lasers had nonthermal impacts on hair growth. The characteristics of cold lasers, according to Posten, et al. are as follows: Output power of lasers is (0.001-0.1) W; wavelengths between (300 and 10,600) nm; pulse frequencies between (0 and 5000) Hz; intensity between (0.01-10) W/cm2 and dosage from (0.01-100) J/cm2 [1,2].
Cold laser radiation is most commonly administered using lasers such as ruby laser (694 nm), argon laser (488 and 514 nm), helium-neon (632.8 nm), krypton (521, 530, 568, and 647 nm), gallium aluminum arsenide (Ga- Al-As) (805 nm or 650 nm), in addition, gallium arsenide (Ga-As) (904 nm) [3].
The application of a laser beam to a biological scheme to endorse tissue regeneration, decrease inflammation, as well as release pain is known as cold laser therapy. Cold laser, unlike other medical laser procedures, doesn't even use an ablative in addition to otherwise a photothermal procedure, but rather a photochemical consequence in which laser is absorbed besides a chemical alteration occurs. The method is termed cold laser therapy because the optimal amount of energy density provided is small, and this is not similar to certain other procedures of laser treatment which are used mostly for ablation; cutting, as well as tissue coagulation [4].
More than a thousand clinical examples of cold laser therapy have been reported worldwide since the foundation of photo biomodulation, photostimulation, low-level laser, or cold laser therapy in the twentieth century [5,6]. Cold laser therapy is a non-invasive laser treatment widely used for the treatment of a variety of physiological health diseases, as well as the therapeutic of incurable wounds, tissues, and nerve abnormalities, as well as the reduction of swelling, fever, and capacity rehabilitation [7].
Laser at (650-1200 nm) has the utmost active tissue penetration, because the chromophores (hemoglobin as well as melanin) have a height band of absorption at a shorter wavelength, in addition, tissue scattering of laser is advanced at a shorter wavelength. Absorption besides a scattering of the lasers in the tissues is considerably higher within the blue section of the spectrum than in the red section [8,9]. Water absorbs the infrared laser at wavelengths ≥ 1100 nm very powerfully. As a result, almost all cold laser therapy in animals in addition to patients uses red as well as near-infrared (600 nm-1100 nm) [10,11].
The laser beam increases the amount of ATP stored energy, which results in increased energy, which speeds up the cell's healing processes. The laser beam also causes arteries and veins around the damage to enlarge, which aids in the removal of cellular debris as well as the increase of nutrients and oxygen [12]. Furthermore, increasing the activity of white blood cells leads to a faster recuperation process. Additionally, certain chemicals that contribute to inflammation are reduced, while helpful antioxidants such as the superoxide dismutase enzyme are elevated [4,13].
Cold laser therapy may be performed in continuous mode or pulsed mode. Modern research has shown that pulsed mode has biological and clinical properties that are distinct from continuous laser mode. While there is an exceptional level of agreement on the most helpful laser wavelengths, as well as typical dosages, there is no consensus on whether continuous or pulsed mode lasers are more appropriate for the many applications of cold laser treatment [14].
It has been reported that pulsed mode is more effective than continuous mode because "quench periods" follow the pulse "on" periods, reducing tissue heating, in addition, to allowing the usage of potentially more power than in the continuous mode [15,16]. This improved power may cause tissues to be heated at the external layers, as well as a pulsed laser could be very useful in this case. For the similar transported energy density, the continuous mode causes a rise in the intervening temperature in addition to target tissues or organs, whereas the pulsed mode causes nonmeasurable alteration in the temperature of the exposed area [17].
It has also been revealed that cold laser therapy in pulsed mode can better penetrate the epidermal barrier, hemoglobin, and melanin, implying that the concept of pulsing was favorable for reaching deeper locations in the tissues and organs [8]. Many recent studies have found that pulsed laser modes are more effective than continuous laser modes, particularly in conditions involving deep tissue restoration and acute management of stroke patients [18]. According to Ilic, et al. a pulsed laser caused no neurological or other damage to muscles, whereas a constant rate of energy transfer caused clear anomalous function of a body area [19].
This article will go forward, but it will not definitively answer numerous questions. How does a pulsed laser differ from a continuous laser in terms of progressing cellular and molecular stages, and what are the implications for cold laser therapy? If the pulsing mode is more appropriate, at what pulse parameters can an ideal result be achieved? What is the ideal frequency or energy density to practice in a hypothetical situation?
Types of laser pulsing generation
Pulsed lasers generate light in the form of optical pulses rather than continuous light. This article review indicates a broader range of pulse-generation than is typically designed for Q-switched, which typically hand on nanosecond. Depending on the duration, the optical energy content of a pulse, pulse repetition frequency, and expected wavelength, quite sophisticated methods for pulse generation, as well as many different types of pulsed, are used. Pumping them required the use of electric pulses of varying lengths [20].
For CO2 lasers employed in high-power, short-duration ablation systems, the idea of super pulsed technology was independently promoted, where heat dissipation limitations narrowed the highest values of energy and this could be applied for stimulating lasing mechanisms. The short pulses produced by CO2 could circumscribe the thermic energy within the tissues by producing a pulse with a shorter duration than diffusion thermal time, reducing the associated thermic damage to normal tissues [21].
A GaAs diode laser, which has a wavelength of 904 nm and pulse duration of approximately 100-200 ns, is another type that has benefited greatly from super pulsing. In-Ga-As diode lasers, which have the same wavelength as GaAs but produce extremely short pulses of 200 ns with high rates of kHz, are also being developed. These pulses have colossal peak strengths of 1-50 W, as well as a typical power of 60 mW [1].
The effectiveness of laser wound therapy in pulsing mode
Because of the pulse on/off times, which results in more limited tissue heating, increased regulations are required in circumstances when light is helpful to reach thicker tissues in order to give enough energy toward goal tissues [22]. The continuous and super-pulsing laser modes both produce helpful laser light, but they transmit it to the tissue in distinct ways. The continuous mode laser produces a steady and stable power output, which is ideal for most treatment scenarios. Except at very high power up to 50 W, super pulsing laser mode uses very short-pulsed energy, barely fractions of a second, to improve laser penetration to deep tissue. By turning on the laser for a brief time at extremely high power, you can have the benefit of deep penetration without the risk of overheating or burning that comes with using higher power, continuous mode laser for long periods of time. Ilic and his colleagues found that a 750 mW/cm2 pulsing laser applied for 120 seconds on an intact rat brain caused nonurological and even tissue damage, whereas the same power density achieved in continuous mode caused marked neurological deficits [19].
The more powerful peak capabilities that may be inadvertently induced when using a pulsing laser may be sufficient to overcome tissue-heating challenges while also improving the laser's ability to reach deeper tissues. The prevalence of pulsed mode support used for cold laser therapy, with frequencies ranging from 2.5 Hz to 100 KHz and pulse durations typically lasting a few milliseconds, provides additional biological evidence for the superiority of pulsed mode light over continuous mode light [23]. Furthermore, this comment implies that if there is a physiological interpretation of processed outcomes of pulsing laser mode, it is because of the unusual frequency or, alternatively, several physiological ways with a sequence level of a few ms.
Fundamental parameters of pulsed laser sources
The following primary parameters are common fundamental conditions of pulsing laser procedures and are critical for assuming larger issues that are forward,
Wavelength of a light beam describes its spatial frequency. It is one of the most important factors in determining the efficacy of cold laser therapy. Depending on where they fall on the spectrum, different wavelengths have different therapeutic effects. Cold laser therapy wavelengths fall into an "optical window" at wavelengths 600-1070 nm as shown in Figure 1. Since the primary tissue chromophores have high absorption at shorter wavelengths, tissue penetration is maximized in this range of 600 nm [24,25]. Wavelengths in the 600-700 nm range are used to treat superficial tissue, while longer wavelengths in the 780 nm-950 nm range are used to treat deeper-seated tissues (Figure 1) [26-28].
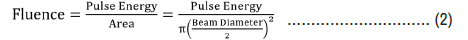
Power and energy are proportional to the average power and inversely proportional to the repetition rate as given by eq.1
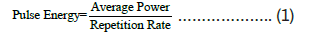
Fluence as opposed to power density. It is necessary to understand that while J/cm2 doesn't include a time unit but the damage threshold is conditioned on pulse duration. The relation between a fluence of a pulsing laser, pulse energy, and the beam diameter is determined through the eq.2
Pulse duration or pulse width is usually described as pulse full width at half maximum of shape.
Repetition rate or frequency represents the number of pulses emitted every second.
Studies comparing the therapeutic effect of continuous and pulsed modes on wound healing
Twenty-two studies on the pulsing mode of low-power laser treatment were investigated in this revision. As shown in Table 1, fifteen of them instantly compared a laser in continuous mode as well as pulsing mode. In twelve of the fifteen studies, the pulsing mode was found to be more effective than the continuous mode. One of these studies comparing continuous mode and pulsed mode laser operation discovered that both modes are regularly effective, with no considerable statistical difference. Furthermore, two of fifteen studies stated that continuous mode produced better results than pulsing mode. One of the recurring requirements of the papers in this study was that the radiation parameters were not used or were not presented in a clear manner. For example, Savolainen, et al., discovered that the continuous mode performed better than the pulsed mode in whole blood coagulation and fibrinolysis, but this is due to the laser mode operation or the laser wavelength that was used, where they used 308 nm in the pulsed mode and 1064 nm in the continuous mode [29].
| References | Focus subject | Laser description parameters | Outcomes |
|---|---|---|---|
| [30] | Mice/traumatic brain injury | 810 nm; pulsed mode 10 Hz; continuous mode 100 Hz, spot diameter 1 cm, power density 50 mW/cm2 for 12 min. fluence 36 J/cm2, duty cycles 50% | pulsed mode>continuous mode |
| [39] | Mice/burns healing | pulsed mode 637 nm; continuous mode 785, 637 nm,1000 Hz;3.5 mw, 2 mw, energy density 3 J/cm2, duty cycles 50% | pulsed mode>continuous mode |
| [32] | Mice/somatic pain | 610 nm-670 nm;850-910 nm;10, 600, 8000 Hz | pulsed mode>continuous mode |
| [40] | Rats/lesions | 1064 nm; energies of 10, 20, 40 J; fluence of 566 J/cm2 | pulsed mode>continuous mode |
| [34] | Rats/wounds healing | 810 nm;10, 100 Hz; pulsed mode at 40 mW/cm2, 22.6 J/cm2, duty cycle 50% | pulsed mode>continuous mode |
| [41] | Humans/wounds healing | 670 nm;10, 25, 50 Hz; 20 mW, energy density 2 J/cm2 | pulsed mode>continuous mode |
| [42] | Rats/bone nodule formation | 830 nm;1 Hz; 500 mW | pulse mode>continuous mode |
| [19] | Rats/intact brain injury | 808 nm; power densities 7.5, 75, and 750 mW/cm2 | pulsed mode>continuous mode |
| [43] | Rabbits/ischemic stroke | 808 nm;100, 1000 Hz; power density 7.5 mW/cm2,0.3 ms (1,000 Hz), 2 ms (100 Hz), average energy 0.9-1.2 J, duty cycle 30%, 20% | pulsed mode>continuous mode |
| [44] | In vitro/glycated catalase | pulsed mode 905 nm; continuous mode 450,530, 638 nm;100 ns | pulsed mode>continuous mode |
| [29] | Human/blood coagulation | pulsed mode 308 nm; continuous mode 1064 nm; 10 W | continuous mode>pulsed mode |
| [18] | Rats/wounds healing | 635 nm;100,200,300,400,500 Hz | continuous mode>pulsed mode |
| [35] | Rabbits/wounds healing | pulsed mode 904 nm; continuous mode 632.8 nm;4,672 Hz; 50 mW; energy density 8.25 J/cm2, pulse duration 200 ns power 10 mW, energy density 1.65 J/cm2 | continuous mode=pulsed mode |
| [45] | Rabbits/wounds healing | 10,600 nm;100, 25 Hz; continuous mode 2 W; pulsed mode 2 W | pulsed mode>continuous mode |
| [38] | Porcine/wounds healing | 10,600 nm | pulsed mode>continuous mode |
According to the findings of the nine studies, the pulsing mode is more useful than the continuous mode. Eight of them involved the in vivo treatment of the following pathologies: Healing from traumatic brain injury and burns, as well as somatic pain and lesions, wound healing, ischemic stroke, bone nodule formation, and intact rat brain. In one study, researchers estimated the effect of laser therapy with different wavelengths in vitro.
Ando, et al. compared the therapeutic effect of 810 nm during continuous and pulsing modes in a mouse in a traumatic brain injury study [30]. The findings of this study show that an 810 nm laser pulsing mode at 10 Hz was largely successful. They recommended 810 nm pulsing mode at 10 Hz over continuous mode at 100 Hz. Levi, et al., looked into the effect of laser beams on burn healing in mice [31]. The results showed that the pulsed mode laser outperformed the continuous mode laser in terms of re-epithelialization and hair follicles.
Sushko, et al. investigated the analgesic action of electromagnetic waves [32]. A red diode with 640 ± 30 nm and an infrared diode with 880 nm ± 30 nm were used to treat acute pain or tonic in mice. They recommended treatment for tonic pain in this experimental study by using a pulsing mode action of red and infrared light with 10,600 and 8000 Hz, which was shown to reduce the twice quantity of pain paw twitching. Furthermore, it had been demonstrated that the highest efficiency in the control of pain syndrome was practical at 10 and 8000 Hz. Furthermore, the effects are affected by the part of the control, wavelength, and mode of therapy [33].
Cold laser therapy begins as a hopeful drug-free and non-invasive biophysical procedure in immunocompromised subjects with the goal of increasing wound healing and decreasing inflammation. As a result, a study was initiated by Keshri, et al., to estimate the photobiomodulation influences concerning diode laser of 810 nm; with 40 mW/cm2 and of 22.6 J/cm2 via pulsing mode at 10 and 100 Hz via 50 percent of the duty cycle; as well as continuous mode [34]. The results of this study were clear; 810 nm at 10 Hz was more effective than continuous mode and 100 Hz at accelerating wound healing; through attenuating cellular proliferation, improving NF-kB, advancing TNF-α), growing (α-SM) as well as (HIF-1α), including reepithelialization when compared to the control groups.
On the other hand, we mentioned Al-Watban, et al. study on the effects of pulsing and continuous modes of 635 nm laser on wounds healing [18].100 Hz had an enhanced result than the other frequencies, but the dealing effects with a continuous mode were better than the pulse frequency. The frequencies of pulsing weren’t established in this study to improve wounds healing when compared to continuous mode. A study conducted by Braverman, et al. and his group on the biostimulation effects of 632.8 nm laser and pulsing 904 nm laser on skin wound healing in rabbits [35]. In terms of wound healing or collagen area, there were no differences; when compared to control tissue, the epidermal enlargement area was greater when the 632.8 nm laser was used, but the difference was not significant. As a result, 632.8 nm and 904 nm alone or in combination-improved tensile toughness through wounds therapeutic could have delivered tissue agents into a systemic circulation, which could have developed toughness on the opposing side as well [36,37].
The influence of the Nd: YAG laser's pulsing mode, 308 nm on whole blood coagulation and fibrinolysis in vitro was less pronounced, while the use of continuous mode 1064 nm with 10 W, found a reduction in reaction and coagulation times after 3, and 6 seconds of 10 ml blood by Savolainen, et al. [29].
A pulsing CO2 laser would be a valuable device for skin ablation and lesions. Lee, et al. investigated the effects of the pulsing mode of CO2 laser on wound healing in porcine skin [38]. The results revealed that reepithelialization, granulation, and fibroblasts in a pulsing manner were significantly higher than those in a continuous mode (Table 1) [39-45].
Studies assessing for using pulsing mode of lasers alone on wounds healing
Seven of the twenty-two studies reviewed matched up to pulsing mode for wound healing among untreated controls, as shown in Table 2. When compared to untreated controls, each study found pulsed cold laser therapy designate more effective in increasing wounds healing. Longo, et al., Studied experimental wound healing in rats and used a GaAlAs laser at 904 nm for 5 minutes daily for 5 days at a frequency of 3000 Hz and an energy density of 3 J/cm2 [46]. They discovered that at these parameters, there was a promoted therapeutic of experimental wounds in microscopic and histological appearance. They didn't, however, detect any effect when the same parameters were applied at 1500 Hz.
| References | Focus subject | Laser description parameters | Outcomes |
|---|---|---|---|
| [46] | Rats/ Wounds healing | 904 nm;1500 and 3000 Hz; power 20 W; power density 5 mW/cm2, 1.5 kHz, 10 mw/cm2, 3 kHz; energy density 3 J; pulse duration 200 ns | pulse mode>controls, just 3000 Hz was effectual in promoting wounds healing |
| [52] | Rats/Wounds healing | 850-910 nm;500, 3000 Hz | pulse mode>control,500 Hz extra effectual |
| [47] | Rats/ Wounds healing | 820 nm;2.5, 20,292, 20000 Hz; 800 mW/cm2,21.6 J/cm2, 360, 45,3, 0.045 ms 2.5,20, 292, 20000 Hz, 90% duty cycle | pulse mode>control, 20, 292 Hz largely effectual |
| [48] | Human/ Wounds healing | 637, 956 nm;8.58,15.6,31.2,78,287, 702 Hz; irradiance 21 W/m2, 55 W/m2,80% duty cycle | pulse mode>control |
| [49] | Rats/ Wounds healing | 890 nm;80 Hz; 75 W, 0.396 J/cm2, 180 ms | pulse mode>control |
| [50] | Rats/ Wounds healing | 890 nm;3000 Hz;2.3 J/cm2, 11.7 J/cm2 | pulse mode>control |
| [51] | Human/ Wounds healing | 820 nm;700 Hz, 8 J/cm2 | pulse mode>control |
El Sayed, et al. used cold laser therapy on partial-thickness wounds in rats to settle on the best parameters for mast cells as well as degranulation inside injured skin, as well as to define the consequence of varying frequencies [47]. This study used an 820 nm pulsing laser at 2.5, 20, 292, and 20000 Hz with 800 mW/cm2 average power density for 27 s and 21.6 J/ cm2 energy densities. They discovered an increase in cell number that was significantly affected by all frequencies. Furthermore, they over and done with that enlarge within cell number was caused by degranulation rather than pulsing frequency.
Schubert, et al. has recommended the use of pulsing lasers to improve therapeutic rate and shorten healing time by using a phototherapy pulsing laser with infrared light 956 nm and red light 637 nm at 15.6 Hz and 8.58 kHz, respectively [48]. Vasheghani, et al. demonstrated that an 80 Hz pulsing 890 nm accelerated a 3rd-burn degree in rats with 0.396 J/cm2 three times per week [49]. The closure percentage of treated burns was considerably higher than that of untreated. Furthermore, Ezzati, et al., confirmed that using a pulsing laser with 890 nm at energy density 11.7 J/cm2 and 3000 Hz on the third degree of burn in rats significantly increased wound closure rate when compared to un-treated burns [50]. Hopkins, et al. promoted the use of pulsing cold laser therapy in vivo by conducting a study in which they applied an 8 J/cm2 for 5 seconds at a pulse rate of 700 Hz (Table 2) [51,52].
According to the findings of the studies, pulsing laser mode may be preferable to the continuous mode in general. This is thought future especially true for wounds healing and dermatology. Alternatively, with patients who require nervous system regeneration or repair, pulsed mode as a single mode may be less effective than continuous mode, and this could probably be described within the tools of performance cold laser therapy that could be creating of cell stimulation or inhibition. Because of the large number of disparate records, it had been difficult to demonstrate any meaningful relationships between pulsing frequency and pathological conditions. While intended for other pulsing parameters, these had been inadequately and unpredictably summarised. It is recommended that researchers summarise the following therapy parameters on a regular basis: peak power, energy density or dosage, frequency, time of irradiation, spot area, mode of irradiation, type of wounds, and why they prefer cold laser treatment over other methods.
The authors declare that they do not seek monetary benefits or individual associations that may have come into play in order to influence the performance described in this article.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref]
[Crossref] [Google Scholar] [PubMed]
[Crossref]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Journal of Blood & Lymph received 443 citations as per Google Scholar report