Research - (2020) Volume 11, Issue 11
Received: 03-Sep-2020
Published:
12-Oct-2020
Citation: Jozani, Zahra Bayat, Saeed Bayanolhagh, Tofigh Mobaderi and Salar Pashangzadeh, et al. “Effect of Hormonal Contraception on
Disease Progression in Women Living With HIV in Tehran, Iran.” J AIDS Clin Res 11 (2020): 823. doi: 10.37421/jar.2020.11.823.
Copyright: © 2020 Jozani ZB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Objective: We conducted the present study to investigate the potential effects of hormonal contraception (HC) on disease progression in women living with HIV (WLWH).
Methods: In a historical cohort study, the demographic, medical, and reproductive profiles of 50 women registered at a referral HIV clinic, receiving hormonal contraceptives, were selected and compared with a matched control group of female patients who had consistent condom use. Disease progression was monitored for nine months, considering the time of CD4 cell count below 200, the time of antiretroviral therapy initiation, HIV-RNA viral load, CD4+ T-cell count, and finally, death.
Results and Discussion: The mean HIV-1-RNA plasma viral loads and mean CD4+ T-cell counts differed significantly in time points among patients using hormonal contraceptives, while no significant changes were observed among condom users. The mean age was 31.34 (21-51) years, and the meantime from diagnosis was four years. In pap smear result, 16% atypical squamous cells of undetermined significance (ASCUS), 9.2% low-grade squamous intraepithelial lesions (LGSIL), and 1.3% high-grade squamous intraepithelial lesions (HGSIL) were found. More regular menstruation cycles were reported during our follow-up among patients using HC (8.7%); we had two unintended pregnancy cases among those patients, only used condoms as contraception. HC discontinuation was associated with adverse effects, lack of partners' support in oral contraceptive pills (OCP) use. Adequate counseling about how to properly take HC decreases rates of discontinuation.
Conclusion: HC has shown no significant effects on disease progression among women using antiretroviral drugs.
Hormonal contraceptive • HIV • women
Based on recent statistics published by UNAIDS in 2017, 17.8 million (15.4 million–20.3 million) women (above 15 years of old) are infected by HIV which more than two million of them live in Asia [1]. In Iran, estimates show that over 90,000 individuals are infected by HIV that includes 26,000 women over 15 years old. Iranian Ministry of Health has reported that among 36,571 infected Iranians, 17% of them are considered young and adult women, and their numbers are increasing at an alarming rate [2].
The prevalence of HIV/AIDS in pregnant women between the ages of 15 and 24 is considered as an index for determining the percentage of infected women in this age group [3]. The third wave of HIV infection in Iran is caused by sexual interaction (intercourse), and increasing trends are considered as a major concern to health authorities that require urgent attention [4].
Sexual transmission of HIV is the primary cause of infection in most women. Although condoms are recommended as the first choice in HIV prevention and other sexually transmitted infections (STIs), certain aspects such as displeasure or women's inability to suggest it to their partners limit its use by couples [5].
Increased access to antiretroviral treatment (ART) has improved the life expectancy amongst WLWH [6]. It is also important to have a reliable contraceptive method that is easy to access, woman-friendly, and does not negatively affect their disease course. Women who plan not to have more than two children are recommended to use a reliable contraceptive method; the absence of such methods will increase the pregnancy rates to an annual percentage of 90. There are no ideal methods, and their side effects are inevitable. Regardless, a combination of the condom and low dose contraceptive pills (LD OCP) is considered as the safest and most reliable method for healthy women [7].
The Pearl Index indicates the effectiveness of contraceptive methods in a hundred cases during a year. This index can also be used in pregnant women whom their HIV condition has a minimum chance to endanger their fetus.
Finding an appropriate method that decreases the unintended pregnancy rate to its minimal chance ensures the mothers' well-being and does not accelerate or interfere with her disease progression and, at the same time, requires a great deal of precision and accuracy [8,9].
Approximately 120 million women are using contraceptive pills or hormones worldwide. Family planning and a contraceptive method that is safe, effective with minimum side effects are always a concern for women. This matter holds higher importance for HIV infected women regarding fetus exposure and hormonal effects on the disease progression. There is no clear or decisive data on contraceptive pills' effects on HIV progression among Iranian women. Some studies in other countries suggest that these hormones will accelerate disease progression; however, some studies support them. This has provided us with an opportunity to conduct the first medical/fundamental research on this group of HIV infected women, and the results can be used as a public guideline.
The study was performed among two HIV positive women groups who use hormonal contraceptives and condoms (dual method) and just condom user. Samples were selected from patients referring to the voluntary and counseling and testing HIV center in Imam Khomeini General Hospital in Tehran. We had a randomized control sample size. Inclusion criteria were as follows: aged 18-50 years old and using oral or oral hormone prophylaxis and condom administration, having a partner, unwillingness to be pregnant, at least for the next year, pass six weeks of delivery in hormone users, no more than 15 cigarettes per day, hypertension less than 160-100, not having a history of ischemic thromboembolism in bacterial endocarditis, not having migraine headache associated with neurological symptoms, not having breast cancer right now, not having diabetes with retinopathy neuropathy, not having acute sarcoid-tumor, and participants matched for age and using Highly active antiretroviral therapy (HAART) during two groups. After obtaining informed consent, participants completed the questionnaire, which was used to determine the clinical, demographical, and epidemiological. The factors affecting the progression of the disease will be examined. Factors affecting the disease include age, getting pregnant, using HARRT drugs and other drugs, smoking or drugs, nutritional status, and infectious diseases. In the second part of this study, HIV positive women who are currently using their own choice of any of the above methods will be used. The positives of these people should be confirmed by their doctor using the ELISA and Western Blotting tests. After obtaining ethical consent, they entered the project, and as mentioned above, the factors affecting the disease were examined, and they were immunologically monitored for 12 months in terms of the rate of progression of their disease. The evaluation of CD4 T cells counted every three months, and the viral load test was performed at the beginning and end at the of the study. Besides, by using the Pap test, changes in cervical cells were investigated at the beginning and at the end of this period at intervals of every six months. Finally, the results of both groups were collected and analyzed by SPSS 16.
Unconditional Latent Growth Models (LGM) was used to model the growth trajectories of CD4 T cells among HIV patients during the treatment period. Furthermore, the LGM extended to multi-groups LGM to study differences in outcome growth trajectory over six months' time period between two study groups, and the Wald test was used for testing invariance of means of latent intercept and slope growth factors across groups. These models were fitted using the Mplus program version 6.12.
The observed repeated measures: cd4.basline, cd4.1, cd4.2, cd4.3, cd4.4, cd4.5, and cd4.6 are the CD4 T cells of the patients measured since the initial stage of treatment to the sixth month at an interval of one months' time period.
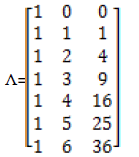
To establishing a linear growth model, the loading to the latent slope growth factor is fixed at 0, 1, 2, 3, 4, 5, and 6 [10] in order to find out the mean value of the initial time point, the factor loading of the baseline assumed to be zero [11]. All the factor loadings to the intercepts were fixed at 1 to indicate means for different months. The quadratic slope growth factor describes the curve is concave up or down. The factor loading for the quadratic slope factor is the squared values of linear time scores. For estimating the quadratic equation model, the following factor loading was used [12].
Our analysis using LGM was powerful to assess features of outcome growth trajectory, such as the initial level, rate of outcome change, and the association between the rate of outcome change and the initial level of outcome change
Model fit and comparison
Chi-square is the most common statistical test used for checking the overall model fit in Structural Equation Modeling (SEM), but it is very sensitive to the sample size [13]. It rejects well-fitted models if the sample size is large, while it does not reject poor models if the sample is relatively small. The other types of model fit indices have been proposed to assess the fit of a model, such as comparative fit indices, which compare the specified model with the baseline model; for example, the Comparative Fit Index (CFI) and Tucker- Lewis index (TLI), the values for CFI and TLI range from 0 to 1. The TLI has a penalty for model complexity because of the more free parameters leading to a smaller TLI. Root Mean Square Error Approximation (RMSEA) is one of the most recently proposed tests measuring overall goodness-of-fit and related to the residual in the model. However, the RMSEA sensitive to the complexity of the model but insensitive to sample size. The two types of information criterion statistics: Aikake information criterion (AIC) [14] and Bayesian information criterion (BIC) [15]. The possible values of AIC and BIC range from 0 to ∞ with smaller values indicating a better fit. The recommended values for adequate fit is defined as CFI>0.9, TLI>0.9, RMSEA<0.08 [16].
In a historical cohort study, the demographic, medical, and reproductive profiles of 50 WLWH registered by the behavioral center were evaluated. Patients receiving hormonal contraceptives were compared with a matched control group of female patients who had consistent condom use.
From 2014 to 2015, we conducted this study among participants who were at least 18 years of age and sexually active. At the time of study enrollment, HIV-1-infected participants had no history of AIDS-defining conditions.
Disease progression was monitored for nine months considering time to a CD4 cell count below 200, the time of antiretroviral therapy initiation, HIV-RNA viral load, CD4+ T cell count, and finally, death.
Volunteers were required to fill a consent form before entering the study; the further survey showed that contraceptive methods are popular among women who were already admitted to the behavioral center before this study.
Subjects were then categorized by their progression stage, which includes CD4 cell counts, viral loads, and their drug treatment programs' effectiveness. CD4 counts were measured every three months, and viral loads were at the beginning and the end of the study; Pap smear was taken every six months to monitor changes in cervical cells.
Data presented by similar researches in this category were mostly focused on cell counts, and factors such as viral load or drug resistance were less significant in them.
Two groups each contain 24 HIV positive women using contraceptive methods, and condoms (double method) and non-use of hormonal contraceptive methods (condom users) were investigated. The demographic characteristics of these individuals are presented in Table 1.
| Variables | Non-Hormonal | Hormonal |
|---|---|---|
| (n=24) | (n=24) | |
| Age, years (mean ± SD) | 31 ± 6.7 | 30 ± 4.1 |
| Job, N (%) | ||
| Unemployed | 21 (87.5) | 18 (75) |
| Employed | 3 (12.5) | 6 (25) |
| Education, N (%) | ||
| Diploma & Upper diploma | 18 (69.2) | 13 (54.6) |
| Under diploma | 8 (30.8) | 11 (45.8) |
| Duration of marriage (mean ± SD) | 19.6 ± 3.6 | 21.1 ± 4.9 |
| Age at first intercourse (mean ± SD) | 18.9 ± 5.1 | 21.2 ± 4.9 |
| Average intercourse (mean ± SD) | 6.7 ± 6.7 | 3.8 ± 2.6 |
| Time from diagnosis (mean ± SD) | 37.6 ± 30.6 | 3.7 ± 4.3 |
| Times AIDS drug Tx (mean ± SD) | 34.8 ± 31.3 | 3.9 ± 3.5 |
The unconditional Linear LGM was fitted for the CD4 of 48 HIV patients (23 condom usage and 25 hormone) and the fit indices were CFI=0.916, TLI=0.923 and RMSEA=0.100. The path diagram of linear LGM is presented in Figure 1. The model fit indices results include AIC, BIC, CFI, TLI, and RMSEA, are presented in Table 2. The change of CD4 of HIV patients during the treatment period was found to be linear because the RMSEA value, BIC, and AIC compared to linear LGMs were increased when a quadratic LGM model of the CD4 was fitted for the 48 patients. In addition, the mean CD4+ T cell number changes in seven different periods are also provided in Table 3.
Figure 1. The linear latent growth model of CD4 change in HIV patients over six months.
| Fit indices | Unconditional Linear | Unconditional Quadratic | Model of 2 groups |
|---|---|---|---|
| (Linear LGM) | |||
| AIC | 4332.26 | 4335.005 | 4315.805 |
| BIC | 4354.715 | 4364.944 | 4360.714 |
| CFI | 0.916 | 0.917 | 0.915 |
| TLI | 0.923 | 0.908 | 0.922 |
| RMSEA | 0.1 | 0.109 | 0.145 |
| Time | Condom (n= 25) | Condom & Hormone (n= 24) | Total (n= 49) |
|---|---|---|---|
| Baseline | 289.76 ± 159.92* | 309.58 ± 220.02 | 299.47 ± 189.96 |
| 1 | 378.28 ± 273.78 | 374.37 ± 175.75 | 376.37 ± 228.66 |
| 2 | 397.36 ± 225.84 | 380.83 ± 171.98 | 389.26 ± 199.36 |
| 3 | 403.88 ± 197.26 | 483.71 ± 257.36 | 442.98 ± 229.82 |
| 4 | 409.00 ± 176.29 | 550.29 ± 393.05 | 478.21 ± 307.66 |
| 5 | 426.24 ± 160.34 | 559.71 ± 265.50 | 491.61 ± 226.22 |
| 6 | 414.84 ± 190.97 | 606.08 ± 278.88 | 508.51 ± 254.62 |
In multi-groups latent growth modeling (LGM), the same LGM was implemented simultaneously for each group. The multi-groups LGM was fitted for compare growth trajectories of CD4 in the condom group, and the hormone group and the fit indices were CFI=0.915, TLI=0.922, and RMSEA=0.145. The model results show that the condom and hormone groups experienced different growth trajectories during the six-month observation period. The observed and estimated outcome growth trajectory is plotted in Figure 2. The results indicate that the initial level of CD4 was a little higher in the condom group (Intercept=339.323 (SE=37.691), p<0.001) than that in the hormone group (Intercept=308.905 (SE=31.779), p<0.001) and the Wald test result (intercepts: χ2=0.381, df=1, P=0.537) indicates that the mean of the initial level of CD4 in the condom group not significantly different from the hormone group. A significant increase in CD4 was observed in the two groups, whereas the increase in the hormone group is higher than the condom group (hormone group: slope=45.981 (SE=8.079), p<0.001; condom group: slope=15.594 (SE=6.443), p<0.05) and the Wald test results (slops: χ2=8.648, df=1, P=0.003) shows that the rate of outcome change over time is significantly different on average between the two groups. It seems no significant relationship between initial level and rate of outcome change in both groups because the covariance between slops and intercepts not significant in two groups (condom group: Cova (Intercept, Slope)= -874.517, P=0.441; hormone groups: Cova (Intercept, Slope)=207.51, P=0.871). In the hormone group, the variances of the intercept and slope non-invariant across samples, and in the condom group, although the variance of intercept non-invariant but variance of slope invariant across samples. Table 4 and Figure 3 show the results and path diagram for twogroup LGM, respectively.
Figure 3. Two-group (a: Condom & b: Hormone group) linear latent growth model of CD4 change in HIV patients over six months.
| Fit Indices | Condom group | Hormone group | Without group | Wald test condom vs. hormone |
|---|---|---|---|---|
| Statistics | Estimate (SE) | Estimate (SE) | Estimate (SE) | X2 (df) |
| Mean | ||||
| Intercept | 339.323 (37.691)*** | 308.908 (31.779)*** | 325.819 (24.948)*** | 0.381 (1) |
| Slope | 15.594 (6.443)* | 45.981 (8.079)*** | 29.373 (5.159)*** | 8.648 (1)** |
| Variance | ||||
| Intercept | 23576.215 (9319.336)* | 17317.162 (6886.3)* | 21070.252 (4673.644)*** | -------- |
| Slope | 441.400 (236.732) | 1277.56 (517.684)* | 1017.739 (346.209)** | -------- |
| Covariance | ||||
| Slope With Intercept | -874.517 (1133.865) | 207.510 (1276.966) | -543.225 (924.903) | -------- |
***P<0.001, **P<0.01, *P<0.05.
The following are researches and studies which both support and contradict the use of contraceptive hormones. A study by Beaten JM in 2007 indicated that contraceptive hormones affect the rate of progression in HIV patients [9]. A study by Stinger E in 2008 indicated that these hormones have an increasing effect on disease progression [17]. Research conducted by Mayer in 2006 on South African women showed that women who used contraceptive hormones have the same risk factor as those who used other methods [18]. Stinger's research on 595 HIV infected women in 2009 showed that the number of women who used contraceptive hormones and Medroxyprogesterone acetate (DMPA) is higher than those who prefer other methods; these women also showed an increasing clinical progression rate compare to those who use nonhormonal methods [19]. A Study conducted by Polis and colleagues in 2010 showed that Combined Oral Contraceptive Pills (COCP) would not endanger the patient's condition and decrease the HIV progression rate [20]. In 2007 Watts conducted a study on 70 HIV positive patients under ARV treatments and showed that using DMPA prevents ovulation, and it will not interfere with viral particle rate and CD4 count [21].
Richardson's study on HIV-infected women showed no variations in CD4 counts and viral loads between hormonal and non-hormonal methods [22]. Some studies suggest hormonal methods will accelerate HIV progression rate; Stinger's research and randomized studies in Kenya and Zambia support this suggestion. Some studies even consider pregnancy and breastfeeding as an acceleration factor for HIV progression [6-19]. In their 2011 study, Morrison and his colleagues concluded that except for older ages, other STDs, and the virus species, hormonal contraceptive methods would not contribute to the AIDS progression rate [23]. Dr. Helkinbeimo's previous experiment in 2009 consisted of three trials. Two of these trials showed that hormonal contraception does not affect the AIDS progression rate; however, one of them resulted in an increased progression rate [24]. Dr. Chelsae's study in 2010 of the effects of contraceptive hormones on women who seroconverted to HIV indicated that these hormones do not affect the AIDS progression rate [25]. There are no reports on the effects of hormones on HIV progression rate in Dr. Curtis's study of the safety of contraceptive hormones and uterine methods in 2009. A randomized controlled trial indicated a high risk of CD4 reduction and mortality rate for hormonal contraception than other methods such as IUDs [26].
Our results are derived using hormonal contraception as dual protection has shown to be acceptable among our participants. Professional counseling is essential to reduce unplanned pregnancies and hence mother-tochild transmission rates. HC has shown no significant effects on disease progression among women using antiretroviral drugs, with consideration to medication contradictions; results indicate that a combination of condom and contraceptive pills is beneficial to patients. The effectiveness of alternative methods is also recommended. Similar studies in Country-level can provide satisfactory results and a superior insight on this matter.
Journal of AIDS & Clinical Research received 5264 citations as per Google Scholar report