Research - (2020) Volume 12, Issue 6
Received: 11-Aug-2020
Published:
14-Sep-2020
, DOI: 10.37421/1948-593X.2020.12.236
Citation: Mariam Dubale, Kaleab Gizaw, Abenezer Aklog, Yitayal Ababu and Lemma Bose. "Treatment Outcome and Associated Factors among Adult Epileptic Patients at Hawassa University Specialized Hospital, Southern Ethiopia.” J Bioanal Biomed 12 (2020) doi: 10.37421/JBABM.2020.12.236
Copyright: © 2020 Dubale M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Epilepsy, once thought to be a disease of evil spirit, is now believed by many as a common neurologic condition that can be effectively treated by optimal use of anti seizure drugs. Despite the availability of multiple and cost effective medications, people with epilepsy could experience episodes of seizures. Aim of the present study was to assess the treatment outcome and associated factors among adult epileptic patients at Hawassa University Specialized Hospital (HUSH), Ethiopia. A cross sectional study was conducted on randomly selected adult epileptic patients. Univariable and multivariable logistic regression analyses were performed to identify factors associated with treatment outcome. Total of 255 patients were included. of whom, 38% had a poorly controlled seizures. Having no formal education [Adjusted Odds Ratio [(AOR): 2.71, 95% Confidence Interval (CI):1.35 -5.46], spending only a year on Anti Seizure Drugs (ASDs) [Adjusted Odds Ratio [(AOR): 4.90, 95% Confidence Interval (CI):1.37-17.50] and low adherence to ASDs [Adjusted Odds Ratio [(AOR): 2.04, 95% Confidence Interval (CI):1.04-4.04] were associated with uncontrolled seizure. Significantly higher epileptic patients had uncontrolled seizure. Epileptic patients with no formal education, who spent a short time on medication and those who have a low medication adherence, were more likely to have uncontrolled seizure. Therefore, more emphasis should be given to these patients.
Treatment outcome • Epilepsy • ASDs • Adult • Hawassa University Specialized Hospital • Ethiopia
Epilepsy the common neurologic condition is a heterogeneous condition characterized by multiple possible seizure types and syndromes, diverse etiologies, and variable prognoses [1].
According to the World Health Organization (WHO), more than 65 million people worldwide suffer from epilepsy with an estimated five million people diagnosed with epilepsy each year. Prevalence in low and middle income countries is estimated to be 139 per 100,000, nearly 3 fold higher than high income countries. Similarly, close to 80% of people with epilepsy live in low and middle income countries [2].
Anti Seizure Drugs (ASD) are the mainstay of epilepsy treatment. The goal of ASD therapy is to eliminate symptoms (e.g., seizures) with minimal side effects. In most patients the goal is complete seizure freedom [3] and up to 70% of people living with epilepsy could become seizure free with appropriate use of anti-seizure medicines. Despite the fact that epileptic seizures are controlled with the optimal use of ASDs, about 33.4% remained uncontrolled even on an optimal therapy [4].
In Ethiopia, according to various studies, the number of patients in whom seizure is not controlled ranges from 17.6% to 71.4% the average being 44% [5-11]. This number is still on the rise despite the availability of modern medications.
Several factors have been found to be associated with treatment outcome in epilepsy. These include; gender, age of seizure onset, type of epilepsy, seizure frequency, etiology of epilepsy, duration of epilepsy, electroencephalography abnormality and presence of co-morbidities [9], alcohol consumption, negative medication belief and low medication adherence, presence of co-morbidities [10]. In contrast, in other studies age older than 20 years at presentation, secondary and tertiary education attainment, being employed, family support, regular clinic attendance and ASD compliance were prognostic factors for better treatment outcome [12]. Poor treatment outcome that is characterized by recurrent seizure while on ASDs may lead to impairment of quality of life, excessive bodily injury from accidents, neuropsychological impairment, social stigma, reduced marriage rates, poor education, reduced employment levels, and finally shortened life expectancy [13,14]
Assessment of epileptic patient’s status of seizure control and problems associated with it is crucial to develop treatment optimization strategies and responsible care of patients as health professionals may face challenges in identifying patients that are less likely to have controlled seizure.
Different studies are conducted in various parts of the world and in Ethiopia regarding the treatment outcome and associated factors among epileptic patients, but there is no adequate data on epilepsy treatment outcome and associated factors in Ethiopia and no study at the study area as a whole since various socio demographic, infrastructural and health professional distribution are variable in different parts of the country. Aim of the study was to assess the treatment outcome and associated factors among adult epileptic patients on Anti Seizure drugs.
Study area and design
The study was conducted at Hawassa University Specialized Hospital, one of the public hospitals in the federal democratic republic of Ethiopia, from February 06 – March 12, 2020. The reason behind choosing the data collection period is because it is a time at which there is more patient flow. A hospital based cross sectional study design was employed through patient interview and chart review to assess treatment outcome and associated factors.
Sample size determination and sampling technique
The sample size to be taken for the study was determined by using the single population proportion formula as follows:
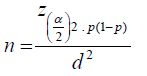
Where, n - sample size zα/2 - confidence interval (1.96) p - estimated prevalence (0.5) d - margin of error to be tolerated (0.05) Based on the above formula and using 95% confidence
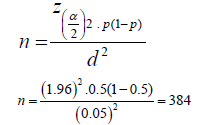
Since the total population is <10,000 the sample was recalculated based on the following formula:

nc = corrected sample size, n = previous sample size (384), N=total number of adult epileptic patients who attend epilepsy clinic of Hawassa University Specialized Hospital (N=592)
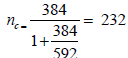 , Therefore the sample size became 232.
, Therefore the sample size became 232.
Considering a 10% contingency for a non-response rate, the final sample size became 255. A systematic random sampling technique was used to select the study population. The procedure of sampling technique is presented in (Figure 1).
Data collection instrument
Data regarding socio demographic, medication use, and triggering factors were retrieved by interviewing patients using a standardized structured questionnaire. Questionnaires were interpreted to the language the respondent listen, understand and speak. Respective medical and medication records were retrieved by reviewing patient’s medical record chart. The clinical information of patients during the last one year follow up period (starting from the date of interview during the data collection period until the last one year) was also assessed.
Assessment of treatment outcome
Treatment outcome was measured in terms of seizure control status and seizure frequency. In order to evaluate epilepsy treatment outcome, seizure status of the patients in the last one year follow up period was also considered. Poor treatment outcome was defined as an increase in number of seizure episode or uncontrolled seizure in patients taking ASDs. If the patient is not seizure free for at least one year it is considered as uncontrolled seizure in the current study.
Assessment of medication adherence
Medication adherence was assessed using Morisky’s medication adherence scale, which has been validated for use in chronic illness adherence assessment. It is a self-reported questionnaire.
Data collection instrument
Data regarding socio demographic, medication use, and triggering factors were retrieved by interviewing patients using a standardized structured questionnaire. Questionnaires were interpreted to the language the respondent listen, understand and speak. Respective medical and medication records were retrieved by reviewing patient’s medical record chart. The clinical information of patients during the last one year follow up period (starting from the date of interview during the data collection period until the last one year) was also assessed.
Assessment of treatment outcome
Treatment outcome was measured in terms of seizure control status and seizure frequency. In order to evaluate epilepsy treatment outcome, seizure status of the patients in the last one year follow up period was also considered. Poor treatment outcome was defined as an increase in the number of seizure episode or uncontrolled seizure in patients taking ASDs. If the patient is not seizure free for at least one year, it is considered as uncontrolled seizure in the current study.
Assessment of medication adherence
Medication adherence was assessed using Morisky’s medication adherence scale, which has been validated for use in chronic illness adherence assessment. It is a self-reported questionnaire which contains eight adherence related questions, in which the total score ranges from 0 to 8 points. The degree of adherence was determined according to the score resulting from the sum of all items. Accordingly, medication adherence was considered as low, medium, and high if the total score is >2, 1-2, and 0 points, respectively (Table 1) [15].
| Questions | Yes | No | |
|---|---|---|---|
| 1 | Do you sometimes forget to take your medication? | ||
| 2 | People sometimes miss taking their medication for reasons other than forgetting. Over the past 2 weeks, were there any days when you did not take your medication? | ||
| 3 | Have you ever cut back or stopped taking your medication without telling your doctor because you felt worse when you took it? | ||
| 4 | When you travel or leave home, do you sometimes forget to bring your medication? | ||
| 5 | Did you take all your medication yesterday? | ||
| 6 | When you feel like your symptoms are under control, do you sometimes stop taking your medication? | ||
| 7 | Taking medication every day is a real inconvenience for some people. Do you ever feel hassled about sticking to your treatment plan? | ||
| 8 | How often do you have difficulty remembering to take all your medication? | ||
| Never/ Rarely 0 | |||
| Once in a while 1 | |||
| Sometimes 1 | |||
| Usually 1 | |||
| All the time 1 | |||
Note - Except question 5, if the patient answers "yes" for the remaining questions, he/she is not adhering to the ASDs. For question 5, it will be counted as non adherence if the patient answers "no". This table is adopted from Source: [15] with modification.
Ethical consideration
Ethical clearance and study approval was obtained from School of Pharmacy, Institute of health sciences, Jimma University. The letter was given to the authorized bodies present at Hawassa University Specialized Hospital where objectives of the study were made clear to the officials.
Permission to interview
the study participants was obtained officially from the administrative office of the hospital. Verbal informed consent was obtained from each participant prior to the interview. Respondents were assured that the information they provided will be kept with a maximal confidentiality and patient initials were only used. The right of respondents to not respond to any of the questions they felt uncomfortable was also respected. In addition, respondents expressed their willingness about sharing of a data obtained from them.
Statistical analysis
Data entry, processing and analysis were performed using Statistical Package for Social Science (SPSS) version 23.0 (SPSS Inc., Chicago, Illinois, USA). A chi square test was employed to identify the potential covariates of treatment outcome at the chronic care unit of Hawassa University Specialized Hospital. The covariate with P-value less than 0.20 by bivariate analysis was retained for the subsequent multivariate analysis. Univariable and multivariable logistic regression analyses were conducted to establish associations between socio demographic, clinical, medication data and treatment outcome. A p value of < 0.05 was considered statistically significant. Data were expressed as frequencies and percentages.
Socio-demographic and clinical characteristics
Two hundred fifty five epileptic patients were interviewed and their medical record data was revised. There were 143 (56.1%) female participants. Majority of patients fall in an age range between 18 and 30 years, accounting for about 70.2% of the total patients. Majority of the study subjects (49.0%) were married and students (34.1%) of all the respondents, 61.9% are rural residents and about 82% of the participants had some formal education. From the total of 255 patients, majorities (64.3%) earn less than 1000 Ethiopian Birr monthly. The most prevalent type of epilepsy was Generalized Tonic Clonic (GTC) seizure in around 60% of patients. Baseline demographic and clinical characteristics of study participants are presented in Table 2.
| Characteristics | Frequency | % |
|---|---|---|
| Age (years) | ||
| 18 -30 | 179 | 70.2 |
| 31-45 | 61 | 23.9 |
| 46-60 | 15 | 5.9 |
| Sex | ||
| Male | 112 | 43.9 |
| Female | 143 | 56.1 |
| Religion | ||
| Protestant | 150 | 58.9 |
| Orthodox | 70 | 27.4 |
| Muslim | 35 | 13.7 |
| Marital status | ||
| Married | 125 | 49 |
| Single | 112 | 43.9 |
| Divorced | 15 | 5.9 |
| Widowed | 3 | 1.2 |
| Occupation | ||
| Student | 87 | 34.1 |
| Merchant | 56 | 21.9 |
| Farmer | 41 | 16.2 |
| Government employee | 35 | 13.7 |
| Laborer | 21 | 8.2 |
| Other* | 15 | 5.9 |
| Residence | ||
| Rural | 158 | 61.9 |
| Urban | 97 | 38.1 |
| Level of education | ||
| No formal education | 46 | 18 |
| Primary | 97 | 38.1 |
| Secondary | 63 | 24.7 |
| University/college | 39 | 19.2 |
| Monthly income (Birr) | ||
| <1000 | 164 | 64.3 |
| ≥ 1000 | 91 | 25.7 |
| Type of seizure | ||
| GTC | 153 | 60 |
| Partial | 36 | 14.1 |
| >1 type | 66 | 25.9 |
| Time on ASDs | ||
| 1 year | 66 | 25.9 |
| 1 - 5 years | 112 | 43.9 |
| >5 years | 77 | 30.2 |
| Comorbid conditions | ||
| Yes | 87 | 34.1 |
| No | 168 | 65.9 |
| Triggering factors | ||
| Yes | 220 | 86.3 |
| No | 35 | 13.7 |
| Electroencephalographic abnormality | ||
| Yes | 22 | 8.6 |
| No | 31 | 12.2 |
| Unknown | 202 | 79.2 |
Note: Other* stands for housewife, retired and private employees
Treatment outcome, medication history and common adverse effects
Among the total population (n=255), ninety seven patients (38%) had a poorly controlled seizure irrespective of the number of antiepileptic drugs prescribed.
Since the major type of epilepsy diagnosed was GTC seizure, the initial ASD prescribed was phenobarbitone in 183 (71.7%) patients, the remaining percentage accounted for phenytoin 53 (20.8%) and sodium valproate 19 (7.5%). Among 183 patients on phenobarbitone, only 49 (26.8%) were seizure free with the initial dose while 134 (73.2%) had no response to the initial dose. Among the 134, dose titration was performed for 93 (69.4%) epileptic patients before adding the second drug.
In addition, 74 patients also took second drugs as an odd on. The most common drug used as add on (second drug) for patients whose seizure is poorly controlled was carbamazepine where 50 (67.6%) patients were on it. In addition, phenytoin and valproic acid were given for 21 (28.4%) and 3 (4.0%) patients respectively. Among patients who used carbamazepine as second drug with phenobarbitone (n=50), 24 of them had their seizure controlled with initial dose of 200mg/day and for 11 patients dose was titrated to 400mg/day, while the remaining 15 patients continued to have seizure despite the dose titration. Among a total of patients on monotherapy (n=181), 124 patients (68.5%) were seizure free with a single antiepileptic drug. Among 74 patients on multiple ASDs, 34 patients (47.3%) were seizure free, while 40 (52.7%) continued to have seizure. The treatment outcome in terms of seizure control is based on the type of medications is presented in Figure 2.
Figure 2. Status of seizure control based on the type of medication among adult epileptic patients on anti-seizure drugs at Hawassa University Specialized Hospital, February 06-March 12, 2020
From the total study population, 129 (50.6%) complained one or more adverse effects from ASDs where 65,38,27 and 6 patients reported side effects for phenobarbitone, phenytoin, carbamazepine and valproic acid respectively. The three most commonly reported side effects were sedation (for phenobarbitone, phenytoin, carbamazepine and valproic acid), confusion (for phenobarbitone and carbamazepine) and gastrointestinal discomfort (for carbamazepine and valproic acid).
Adherence to ASDs and reasons for non-adherence
Using the accepted criterion of a score of Morisky’s 8 item of medication adherence questionnaire, more than half of the total study participants, 137 (53.7%) of them were classified as non-adherent to medications. The most common reasons for non-adherence are described in Table 3.
| Factors related to non-adherence | ||
|---|---|---|
| Frequency | % | |
| Patient related factors | ||
| 119 | 58.3 | |
| Forget to take medication | 25 | 12.2 |
| The schedule of work makes it impossible | 44 | 21.6 |
| Do not believe in the medication due to local beliefs | ||
| Cannot afford to buy the medications | 16 | 7.9 |
| Health professional/ health care system related | ||
| Poor relationship between patient and physician | 19 | 45.2 |
| Irregular or poor drug supply | 14 | 33.4 |
| Long distance from treatment setting | 9 | 21.4 |
| Medication related factors | ||
| Feeling worse/Side effects | 99 | 59.6 |
| Polypharmacy (drugs are too many) | 37 | 22.3 |
| Duration and previous treatment failures | 30 | 18.1 |
Note: The percentage for each reason was calculated from patients who were not adherent (medium adherence and low adherence) (n=137). The percent of each factor was calculated from the total responses provided for each category. I.e. a single patient may report > 2 factors.
Treatment outcome and associated factors
Factors associated with treatment outcome are presented in Table 4.
| Variable | COR (95% CI) | p-values | AOR (95% CI) | p-values |
|---|---|---|---|---|
| Age of the patient | ||||
| 18-30 | 1 | 1 | ||
| 31-45 | 1.50 (0.83–2.70) | 0.17 | 1.37 (0.72–2.62) | 0.33 |
| 46-60 | 1.25 (0.72–2.16) | 0.42 | 1.14 (0.62–2.09) | 0.66 |
| Educational status | ||||
| College/University | 1 | |||
| Secondary | 1.15 (0.45–2.95) | 0.77 | 1.12 (0.42-2.95) | 0.81 |
| Primary | 2.44 (1.39-4.27) | 0.002 | 1.77 (0.94-3.31) | 0.07 |
| No formal education | 3.55 (1.82-6.93) | <0.01 | 2.71 (1.35-5.46) | 0.005* |
| Type of seizure | ||||
| GTC | 1 | 1 | ||
| Partial | 4.04 (1.73-9.45) | 0.001 | 2.25 (0.90-5.63) | 0.08 |
| >1 type | 4.09(1.48-11.31) | 0.007 | 2.74 (0.26-28.4) | 0.39 |
| Time on AEDs | ||||
| >5 year | 1 | 1 | ||
| 1-5 years | 1.15 (0.49–2.69) | 0.72 | 1.62 (0.58-4.57) | 0.13 |
| 1 years | 2.59 (0.98–6.8) | 0.05 | 4.90 (1.37-17.50) | 0.014* |
| Triggering factors | ||||
| No | 1 | 1 | ||
| Yes | 1.97 (0.20-19.50) | 0.56 | 2.74 (0.26-28.4) | 0.39 |
| Adherence | ||||
| High adherence | 1 | 1 | ||
| Medium adherence | 2.44 (1.39-4.27) | 0.002 | 1.77 (0.94-3.31) | 0.07 |
| Low adherence | 2.87 (1.51-5.45) | 0.001 | 2.04 (1.04-4.04) | 0.03* |
| Drug side effect | ||||
| No | 1 | 1 | ||
| Yes | 2.37 (1.25-4.51) | 0.009 | 1.97 (1.01-3.84) | 0.60 |
Note: Asterisk (*) shows significant difference.
The present study aimed to study the magnitude of treatment outcome and associated factors among adult epileptic patients that are on antiepileptic drugs. Major findings of the study are as follows:
38% of study participants had poorly controlled seizure.
Most patients were on monotherapy where 68.5% of the patients were seizure free with a single antiepileptic drug.
More than half (50.6%) of patients complained one or more adverse effects from ASDs.
Significantly higher (53.7%) patients were non adherent to ASDs.
Factors associated with uncontrolled seizure were having no formal education, spending only a year on ASDs and low medication adherence.
Poor treatment outcome is defined as an increase in number of seizure episode or uncontrolled seizure in patients taking ASDs. According to the present study, poor treatment outcome was defined as a failure of being seizure free for about a year. Accordingly, 97 (38%) of patients had a poorly controlled seizure irrespective of the number of antiepileptic drugs prescribed. This number is higher than studies conducted in few countries. The following studies indicate a better statistics from the present study. The prevalence of poor treatment outcome in Scotland (36.3%) [16] and Ethiopia (17.6%) [5] was less than that obtained in the present study. This could be attributed to less qualified medical personnel, unavailability of medications, poor community knowledge and awareness, and non-adherence to their medication in the study area. This number is lower than study conducted in Ethiopia by [10] (38.8%) and [7] (43.3%). This could be due to a better drug adherence profile of patients when compared to the above studies.
Nearly half (50.6%) of study participants complained one or more adverse effects from ASDs where most of the side effect was attributed to phenobarbitone. The most commonly reported side effects were sedation, confusion and gastrointestinal discomfort. These side effects are similar to one study reported by [17]. The reason for this similarity is due to the fact that phenobarbitone was the drug of choice to control seizure in developing countries.
In the present study, most patients were on monotherapy (71%). This number is larger than a study conducted by [10], (48.5%), [18] (44.6%), and [7] (54.5%). This is particularly important in that most patients were on monotherapy which is believed to reduce side effect due to combined drugs and non-adherence due to pill burden and financial expense.
Adherence to drugs is a critical and crucial issue towards bringing about good treatment outcome in every medical problem. Failure to do so can lead to the opposite. Accordingly, in the present study more than half of study participants (53.7%) were found to be non-adherent to their medications. This finding is higher than studies conducted in Sudan (35%) [19], Yirgalem Hospital, Ethiopia (32%) [20] and Amanuel specialized hospital, Ethiopia (30%) [11]. The reason for the higher number in the present study could be attributed to a large number of study participants that either have no formal education or are in primary school. In addition, low adherence to ASDs [Adjusted Odds Ratio [(AOR): 2.04, 95% Confidence Interval (CI):1.04- 4.04] was also associated with poor treatment outcome in the present study. This is also evidenced in some studies [9,10]. In another study conducted in Nigeria, it was discovered that adherence to ASDs was associated with better prognostic factor in patients in whom seizure is controlled [12].
The most common reasons for non-adherence in the present study were forgetfulness, feeling worse/side effect of the drug and failure to believe in the medication because of local beliefs. Similar to this finding, in most studies conducted in Ethiopia, the leading causes of non-adherence was forgetfulness [20,21], safety concern [21]. In all studies, including ours, forgetfulness was the main reason for non-adherence. This challenge should be eliminated or reduced by creating awareness for epileptic patients and creating a way for patients to use reminders or alarm clock to reduce such a problem because it is a modifiable reason.
Having no formal education was one of the factors associated with poor treatment outcome [Adjusted Odds Ratio [(AOR): 2.71, 95% Confidence Interval (CI):1.35 – 5.46]. This finding is similar to a study conducted in Amanuel hospital where educational level was found to have a significant association with treatment outcome [11]. In another study conducted in Nigeria, it was discovered that secondary and tertiary education attainment was associated with better prognostic factor in patients in whom seizure is controlled [12].
Spending only a year on ASDs [Adjusted Odds Ratio [(AOR): 4.90, 95% Confidence Interval (CI):1.37-17.50], was associated with poor treatment outcome. This finding is new and no other study found an association between stay on ASDs and treatment outcome. This finding can be explained by the fact that patients that have less experience on medications are not going to adhere to medications and this by itself can lead to poor treatment outcome.
Significantly higher number of patients had a poor treatment outcome. In addition, more than half of the study participants were not adherent to their medications due to different reasons. Factors associated with poor treatment outcome were being illiterate, being on ASDs for about a year and low adherence to ASDs. Since there are no studies conducted in the study area regarding treatment outcome, further studies are needed to evaluate the effect of adherence on seizure control and other associated factors that may contribute to poor treatment outcome among epileptic patients.
The present study is not without limitations. The data collection period is short. The number of study participants is small to generalize. Therefore, we suggest future researchers to collect data from larger population size over a long period of time. In addition, future researchers should incorporate additional statistical analyses to discover additional factors that could be associated with poor treatment outcome.
We would like to express our deepest gratitude and appreciation to the study participants for giving their precious time in collecting the data. We would also want to thank data collectors and administrative staffs of Hawassa University Specialized Hospital.
Journal of Bioanalysis & Biomedicine received 3099 citations as per Google Scholar report