Case Report - (2020) Volume 6, Issue 2
Received: 28-Jun-2020
Published:
17-Jul-2020
Citation: Diarra Abdoulaziz, Diallo Ahmad Moustapha, Guirassy
Mouhamadou Lamine, and Kane Aboubacar Sidiki Tisse, et al. “Periodontal
management in a periapical osseous dysplasia context: A case report.” Oral
health case Rep 6(2020) 1-6. DOI: 10.37421/ohcr.2020.6.3
Copyright: © 2020 Diarra A, et al. This is an open-access article distributed
under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited.
Introduction: Osseous dysplasias are benign fibro-osseous lesions in the group of non-odontogenic tumors of the maxillae. Periodontitis is an inflammatory pathology of multifactorial origin, which destroys the attachment system of the tooth. By its main etiological factor (dental plaque) and its evolution, periodontal disease constitutes comorbidity in osseous dysplasia and exposing the patient to an infectious risk. The objective of this work was to present, through an illustrated clinical case, a periodontal therapeutic approach in a patient with periapical bone dysplasia.
Case Report: A 57-year-old woman, referred by her dentist for periodontal treatment, presented to our service with the chief complaint “loose teeth and presence of inter-dental spaces”. The clinical examination and the paraclinical assessment made it possible to make the diagnosis of severe generalized chronic periodontitis associated with periapical osseous dysplasia. Periodontal treatment has been instituted. Surveillance has been established for the dysplastic lesion.
Conclusion: This case report illustrates the management of severe chronic periodontitis in a patient with OD. We focused on the non-surgical therapeutic approach in the mandibular anterior area with OD, completed by open flap debridments on posterior sites, resulting in a significant reduction in the percentage of sites with attachment loss greater than or equal to 5mm and stabilization of periodontal disease.
Osseous dysplasia; Chronic periodontitis; Periodontal therapeutic
Osseous dysplasias (OD) are benign fibro-osseous lesions in the group of non-odontogenic tumors of the maxillae [1]. They are part of a set of entities within which the normal architecture of the bone is transformed into metaplastic bone, composed of fibrous tissue associated with a cementoid mineralized substance in variable proportion [2]. OD can occur at all ages and in all ethnic groups, with high prevalence (90% of cases) in black or asian women in their fifties without any scientific explanation [3,4].
OD take on various clinical and radiological aspects. According to the World Health Organization (WHO), three forms of lesions sharing the same histopathological process are found: periapical, focal and florid [5]. The periapical and focal forms are the most frequent [6]. These two forms are characterized by lesions of reduced size, localized, interesting a small number of teeth [7]. Usually asymptomatic, OD is discovered fortuitously during a routine radiographic examination [8].
Periodontitis is an inflammatory pathology of multifactorial origin which destroys the attachment system of the tooth. It is a real public health problem according to the WHO, which considers it to be the 6th epidemiological plague in the world [9]. By its main etiological factor (dental plaque) and its evolution, periodontal disease is an infectious risk factor in the presence of OD.
The objective of this work was to present, through an illustrated clinical case, a periodontal therapeutic approach in a patient with periapical OD.
Ms. SB. 57-years-old, referred by her dentist for periodontal treatment presented with as main complaint “loose teeth and presence of inter-dental spaces”. The anamnesis revealed the presence arterial hypertension followed and treated under Detensiel, harmful food habits (nibbling) and the use of the toothbrush stick as a complementary mean of oral hygiene. Dental and occluso-functional examinations revealed occlusal caries on 17-28, coronary restorations and multiple non-carious cervical lesions, the uncompensated absence of 36, the egression of 26, the versions of 21-27 and finally excessive overlap and overhang in the anterior sector (Table 1).
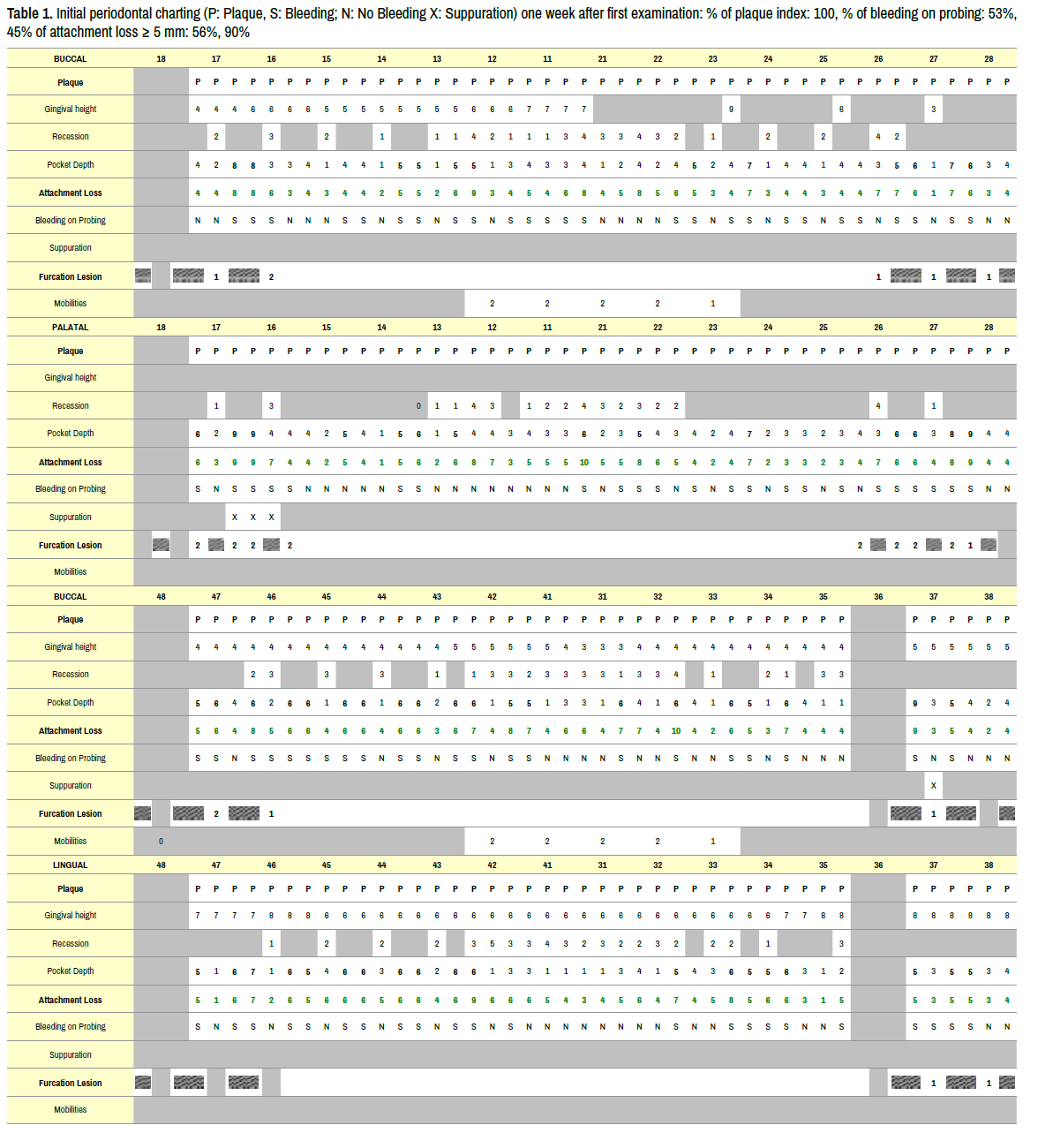
On periodontal examination, the patient presented signs of generalized plaque and bleeding (100% and 53.45% respectively), a gum spotted with melanic deposits of normal volume with a flat and thick biotype and presenting inflammatory exudates on probing. We observed, around 57% of sites with a pocket depth superior or equal to 5 mm, multiple Miller class III recessions.
Muhlemann type 2 dental mobility in the anterior sectors and furcation lesions on all molars. The deep periodontal examination is summarized in Figure 1. The additional radiographic examination revealed:
The presence of generalized horizontal bone loss around the third medium of the root with a vertical variant on the mesial faces of 22, 24, 37 and on the distal face of the 46 (Figure 2a). - The presence of a circumferential lesion around 12 and 16 (Figure 2b). - The presence of periapical lesions of mixed appearance associating radiopaque and radiolucent images at the level of the anterior mandibular sector. A more in-depth investigation was carried out by performing a Cone-Beam Computer Tomography (CBCT) localized to the anterior mandibular region (Figure 2c). All the teeth related to these lesions were vital and asymptomatic. The diagnosis of severe generalized chronic periodontitis was made [10] associated with a Dento-Maxillary Dysharmony (DDM) in a field of mandibular periapical osseous dysplasia. The following treatment plan was offered to the patient:
Figure 2. Radiograph examinations
(a) Orthopantomogram performed during the first consultation,
(b) Periodontal status showing periodontal bone defects and heterogeneous periapical mandibular lesions (red arrow) one week later
(c) CBCT sagittal and axial slices of the anterior mandibular sector objectifying dysplastic lesions performed before starting non-surgical therapy.
Non-surgical periodontal therapy with the aim of improving plaque control and stopping inflammation: Motivation and teaching in oral hygiene, Scaling Root Planning,
Antibiotherapy: Amoxicillin 1 g × 2/day + Metronidazole 250 mg × 3/day for 14 days + Chlorhexidine 0.12% in mouthwash after brushing for 14 days) (Figure 3). Periodontal re-evaluation two months after non-surgical therapy [11] (Table 2).
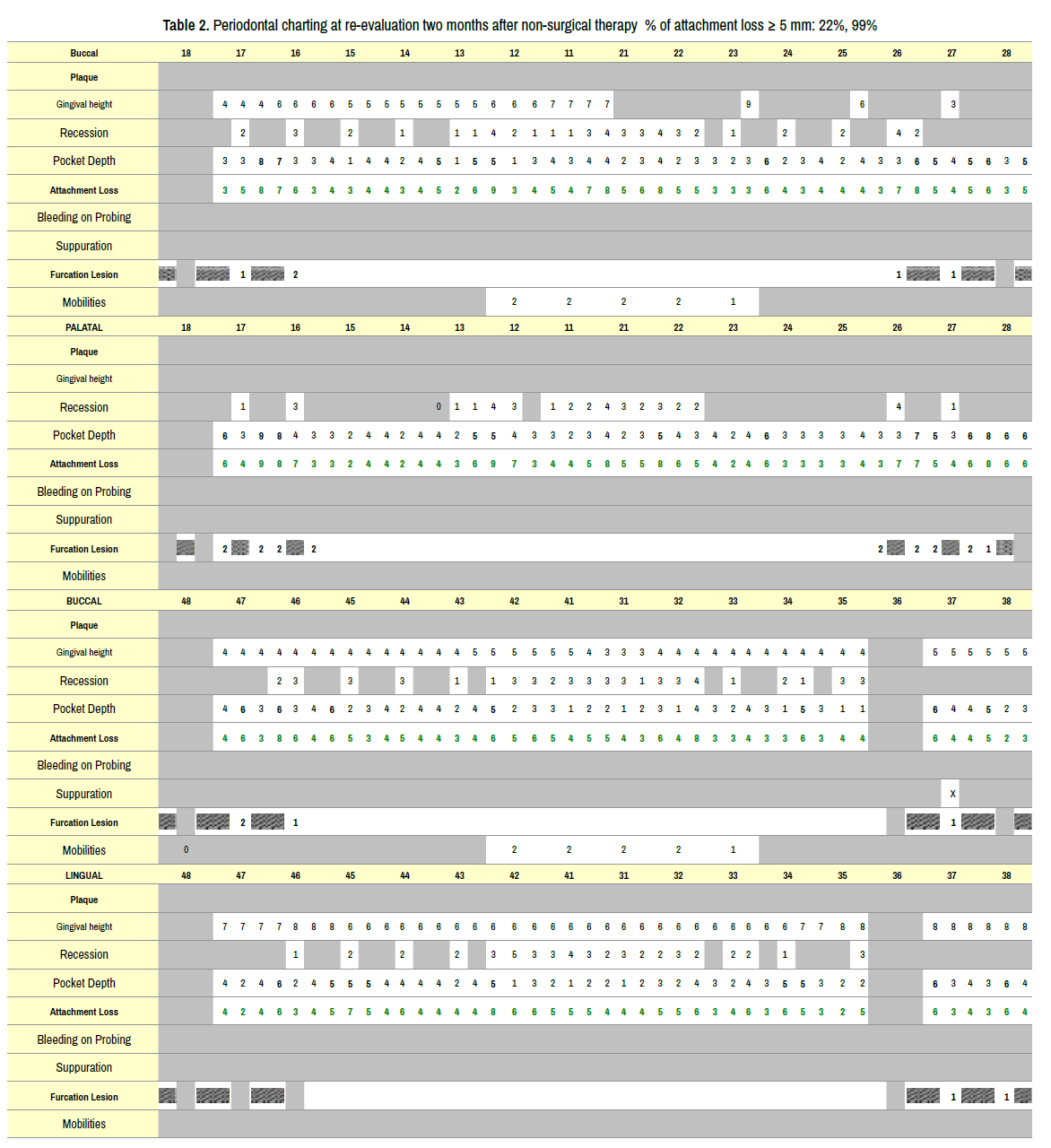
Surgical therapy: open flap debridement in posterior sectors in order to stop attachment loss to remove the residual periodontal pockets [12] (Figure 4).
Proposal therapy: Orthodontic treatment for diastema closures, incisor block intrusion and reduction of recessions; Development of prosthetic spaces and dental implant replacing 36. Periodontal support therapy every six months.
Our work illustrates the management of severe chronic periodontitis in the context of periapical OD and aesthetic damage. Periodontal disease is an infectious risk factor in the presence of OD. Indeed, periodontitis can constitute a microbial entry door capable of causing a secondary infection of the dysplastic lesion. The patient presenting a severe case, a stabilization of the periodontal state by a control of the inflammation and a global periodontal debridment was essential.
This contributed to improving the prognosis of the antero-inferior teeth, the extraction of which could lead to activation of the dysplastic lesions and and also interradicular lesions of the underlying molars.
Surgical abstention was observed at the antero-inferior level, despite the 5mm distal pocket persistance of 42, in order to remain less invasive as possible. The poorly vascularized dysplastic tissue is very susceptible to infections [13]. Any invasive act in the dysplastic zone therefore constitutes a risk of the appearance of an extensive infection progressing to osteomyelitis, or even the formation of a bone sequestration [8].
Periodontal care is also preventive in this context. It not only helped to stop periodontal disease in the patient, but also minimize the incidence of periodontal pockets and possible dental avulsions on the infectious complications of dysplastic lesions.
The pathogenesis of OD is unknown [14]. Some authors suggest an involvement of the osteo- progenitor cells of the alveolo-dental ligament, hence the localization of the OD in the peri-apex [15]. Others suspect a defect of bone remodeling influenced by local factors or a hormonal imbalance [2]. Involvement of the medullary bone has also been mentioned [16].
OD can present multiple radiographic aspects [16]. Indeed, the lesions are progressive over time the consequence being a progressive substitution of the fibrous portion of the bone by a mineral portion [2,13]. This substitution takes place in three successive phases: an initial phase in which the resorption of normal bone and the deposition of fibrous tissue results in the development of well-defined periapical round or ovoid radiolucencies associated with punctate radiopacities. Then appear mixed lesions characterized by the development and coalescence of crimped radiopaque masses, of a radio-clear halo; these so-called "target" lesions result from progressive intralesional sclerosis; and finally mature lesions, which can be completely opaque; these are dense, lobulated and confluent sclerotic masses.
The odontologist plays an important role in the diagnosis of OD. Depending on the aspect and the stage of development of the lesion, the differential diagnosis varies and must be made with regard to other benign maxillary tumors (cystic lesions) and other fibro-osseous lesions (particularly fibrous dysplasia and ossifying fibroma) [7].
The absence of an extra-oral skeletal anomaly, biochemical disturbances or systemic manifestations generally allows an initial diagnostic orientation. It is the practitioner’s responsibility to familiarize him with the various clinical and radiographic aspects of the other lesions in order to establish the correct diagnosis and avoid inappropriate surgical intervention [7]. In addition, biopsies are not necessary to establish the diagnosis and can cause serious healing delays [15]. In the absence of clinical symptoms, no treatment of the dysplastic lesion should be undertaken.
Therapeutic abstention and surveillance seem to be the rule, especially since some authors report difficult surgical procedures as well as post-operative complications [17]. Indeed, Chang- Ki and co. in 2018 reported during periodic follow-up, a persistence of symptomatology and a recurrence of lesions after surgical treatment of OD [18].
In the presence of toothlessness, the removable prosthesis is not recommended. It could generate an undesirable alveolar bone resorption and constitute a traumatic agent, which could lead to a breach of the mucous barrier hence the proposal of implant to the patient [15].
The implant placement is not unanimous. A risk of osseointegration failure remains possible in the face of this abnormal and poorly vascularized bone associated with a risk of exposure of dysplastic zones during the intervention [18]. Bencharit et al. in 2003, however, reported a successful implantsupported prosthetic rehabilitation [19]. These difficulties thus related to the managment and prosthetic rehabilitation reinforces the need to preserve and maintain natural teeth on the arch.
The consequences of an orthodontic movement in the context of OD are poorly documented. The possibility of performing orthodontic treatment should be discussed according to the benefit/risk ratio of the treatment. In all cases, treatments requiring tooth avulsion in connection with the lesions should be avoided [20].
This case report illustrates the management of severe chronic periodontitis in a patient with OD. We focused on the non-surgical therapeutic approach in the mandibular anterior area with OD, resulting in a significant reduction in the percentage of sites with attachment loss greater than or equal to 5mm and stabilization of periodontal disease. In addition, the open flap debridments eliminated residual periodontal pockets.
Our study, however, has some limitations. It is a clinical report about a one case that does not allow the generalization of the results obtained. It would have been interesting to have a radiological follow-up over time in order to better appreciate the effect of non-surgical therapy on OD.
Conservative therapy is an approach to be favoured in the management of such patients while emphasizing the preventive aspect to avoid the establishment of an infection. Dental surgeons and periodontists in particular, must ensure the maintenance of good oral and periodontal health because this not only limits the risk of tooth loss and infectious complications but also guarantees a good prognosis for these patients.
Oral Health Case Reports received 120 citations as per Google Scholar report